Did you know?
- 32% of all U.S. opioid overdose deaths involve a prescription opioid.1
- An average of 41 people die every day from overdoses involving prescription opioids.1
Recent statistics paint a pretty scary picture of the growing opioid epidemic in the United States, especially concerning prescription opioid misuse and abuse. In spite of the emerging research and reported trends, it can be easy to get confused by commonly believed myths. If you are prescribed opioid medications, it’s important to be aware of myths and understand the real facts so you can be a responsible patient and ensure you don’t contribute to the opioid crisis.
 MYTH: If I am prescribed an opioid painkiller, there must be no other treatment options.
MYTH: If I am prescribed an opioid painkiller, there must be no other treatment options.
FACT: Opioid medications are only one of many options available for pain management. Opioids are typically best for short-term/acute pain management (such as after a surgery or injury), but they’re not as effective for long-term/chronic pain. Depending on individual circumstances, an opioid prescription may be the best choice. However, you should always discuss other possible options with your healthcare provider. Other options for treatment may include physical therapy, lifestyle changes such as exercise and weight loss, acupuncture, massage or other medications like Acetaminophen or Ibuprofen.2
MYTH: I cannot become addicted to a prescription my doctor gives me.
FACT: You CAN become addicted to opioid medications, even if they were prescribed by a doctor. It is a common misperception that if a medication is prescribed by a doctor, it is totally safe and non-addictive. However, many prescribed medications are highly potent and have the potential for addiction.3 While misusing these medications leads to a greater chance of addiction, addiction is still a risk, even when they are used as prescribed. Anyone can become addicted to prescription opioids. Anyone can also develop tolerance (needing to take more of the same medication over time for the same relief) or dependence (experiencing withdrawal symptoms when the medication is stopped).4 Research has shown that many factors can increase a person’s risk of addiction such as depression, anxiety, other psychiatric illnesses and a history of substance abuse. Everyone should discuss their medical history and any concerns with their doctor before beginning a treatment that involves opioids.5
MYTH: I should always finish all of the prescription painkillers my doctor prescribed.
FACT: Opioid medications should only be used until they are no longer needed. If you’ve been sick before, you’ve probably been told by a doctor or pharmacist to continue taking your antibiotics until they’re all gone, even after you’re feeling better. While this is true for antibiotics and some other medications, it is definitely not true for painkillers. Risk of opioid overdoses and death increase at higher dosages and when taken for longer periods of time.4 Once you feel better and no longer need them for their intended use (such as for pain after a car accident or surgery), you should discontinue taking them. Remember that these types of medications are best for short-term/acute pain, and doctors should only prescribe them in small dosages as a part of a very time-limited treatment schedule.
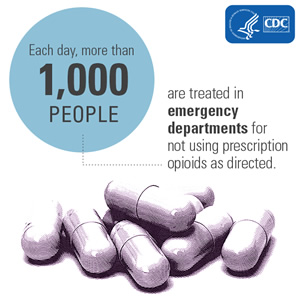 MYTH: It is okay to share my prescription medication with close a friend or relative.
MYTH: It is okay to share my prescription medication with close a friend or relative.
FACT: You should never share any prescription with another person, especially an opioid medication. Only an individual’s doctor should recommend and prescribe medications, as they have the proper training that allows them to determine the right medication, dosage and treatment schedule to treat a particular issue. Doctors also consider important factors such as medical history when prescribing a medication. Most people who abuse prescription opioids get them from a friend or relative. Of those who are at the highest risk of overdosing, only 15% obtain prescription opioids from a drug dealer.6 These alarming statistics are proof that this issue is a lot closer to home than we think. With the growing opioid epidemic, it is important now more than ever to ensure we are doing everything we can to prevent prescription drug misuse. You can review these helpful tips for how to do your part at home.
Want more information? Suggestions on how to prevent opioid misuse are available here. You can also find helpful materials for patients with acute and chronic pain here.
Updated 9/10/20
Sources:
- https://www.cdc.gov/drugoverdose/data/prescribing/overdose-death-maps.html
- https://www.cdc.gov/drugoverdose/patients/options.html
- https://drugabuse.com/library/drug-addiction-facts-myths/
- https://www.cdc.gov/drugoverdose/patients/faq.html
- https://www.consumerreports.org/cro/2014/01/5-surprising-things-you-need-to-know-about-prescription-painkillers/index.htm
- https://www.cdc.gov/media/releases/2014/p0303-prescription-opioids.html